

Northern CaliforniaWomen's
Imaging Center
141 California Ave, B202 (2421 Park Blvd, B202)
Palo Alto, CA 94306
(650) 617- 8655

Biopsies: Why And What To Expect.
Suspicious areas detected on mammography or ultrasound may require a biopsy to determine if the lesion is benign (not cancer) or cancerous. Biopsies can be performed by surgical or non-surgical approaches. Non-surgical approaches are also called core biopsies and are less invasive than surgical approaches. For this reason, the core biopsy procedure is the preferred method of choice.
The results of the biopsy can not be determined at the time of the biopsy. Once the tissue is removed, the sample(s) are sent to the pathology department to classify and characterize the tissue.
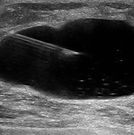
What is an ultrasound guided cyst aspiration?
When a complex cyst is identified within the breast at the time of ultrasonographic evaluation then further evaluation with a cyst aspiration may be warranted. During the cyst aspiration procedure, the patient will lie on her back, the breast will be cleansed and a small amount of local anesthesia administered. Then, a small needle will be introduced into the the breast to remove the fluid within the complex cyst. If the fluid is unable to be removed or the fluid removed has a concerning appearance, then further evaluation with an ultrasound guided core biopsy would be performed. If the fluid drained from the cyst has a suspicious appearance, then further characterization of the fluid from the cytology lab may be indicated.

What is an ultrasound guided breast biopsy?
When a suspicious abnormality is best seen on ultrasound, then further evaluation with an ultrasound guided core biopsy is often recommended. The core biopsy technique uses a small hollow needle to take samples of the breast while using ultrasound to identify the target and provide guidance during the procedure. During the ultrasound core biopsy, patients lie on their back; after cleansing the breast, a small amount of local anesthesia is administered to minimize any discomfort. A small hollow needle is then placed into the breast with ultrasound guidance and a few samples of breast tissue are retrieved and sent to the pathology lab for further characterization.

What is Stereotactic guided breast biopsy?
If a finding is best seen on mammography and is found to be approachable with a needle biopsy then further characterization of the lesion with a stereotactic biopsy may be recommended. This is commonly performed to evaluate developing clusters of microcalcifications but can also be performed for other findings.
During a stereotactic breast biopsy, a specially designed examination table will allow the patient to lie face down with her breast hanging freely through an opening in the table. The table is then raised and the biopsy procedure is performed beneath the table. The breast will be cleansed and a small amount of local anesthesia delivered to minimize discomfort. A special mammography machine uses x-rays to pinpoint the area of concern in all three dimensions. The radiologist is then able to target the area of concern with a hollow needle and remove small samples of tissue.
Stereotactic biopsies can be limited when lesions are found in areas of the breast which are not approachable or if the breast tissue size and contour are not adequate. At NCWIC, we use the state of the art Hologic Eviva device which quickly removes tissue and often allows for core biopsies to be performed in women with smaller breasts who traditionally, would require surgical excision.

What is wire or SAVI localization?
When an area of concern in the breast cannot be safely or accurately biopsied with a core needle, or when a core biopsy shows a high-risk lesion or cancer, surgical evaluation may be recommended. Before surgery, the area often needs to be precisely marked to help the surgeon remove only the tissue in question.
Traditionally, this is done with a needle localization procedure, where a thin wire is placed into the breast by the radiologist to guide the surgeon directly to the spot of concern. Needle localization can be performed using either mammography or ultrasound guidance:
-
With mammographic guidance, the patient typically lies on her stomach while the breast is gently compressed for imaging.
-
With ultrasound guidance, the patient lies on her back, and the breast is not compressed.
-
In both cases, the breast is cleaned, numbed with local anesthetic, and carefully imaged so the wire can be placed accurately. Imaging confirms the placement, the wire is secured, and the needle is removed, leaving only the wire in place for surgery.
We also offer SAVI Scout® localization, a newer, wire-free option. In this procedure, a tiny reflector about the size of a grain of rice is placed in the breast at the area of concern, often days before surgery. During surgery, the surgeon uses a special detector to locate the reflector and remove only the targeted tissue. SAVI Scout can make the day of surgery easier and more comfortable because no wire placement is needed that morning, and it allows more flexibility for both patients and surgeons.
Both traditional wire localization and SAVI Scout localization are highly accurate tools to ensure safe, precise breast surgery while removing as little tissue as necessary.

How do I prepare?
Before the procedure:
We request that you discontinue any "over the counter" blood thinners (including aspirin or ibuprofen products such as Bayer aspirin and Advil) one week prior to the biopsy. If you are routinely prescribed blood thinners such as coumadin for other known health conditions, please consult with the prescribing physician prior to the biopsy and inform the NCWIC staff. Additionally, please let us know if you have any known allergies or reactions to medications or anesthesia.
Eat and drink as you normally would.* Wear comfortable clothing. Inform the breast center if you have excessive coughing or other reasons why it would be difficult for you to remain recumbent and still during the procedure.
After the procedure:
You should avoid strenuous activity for 24 hours after returning home, but then usually you will be able to resume normal activities.
You should contact your physician if you experience excessive swelling, bleeding, drainage, redness or heat in the breast.
*These guidelines are specifically for radiologic procedures. Please speak to your surgeon regarding preparation for any surgical procedures.